 While talking recently with a colleague from NAMI Colorado, Array Parity project leader Max Maddox was introduced to Dr. Melba Arnold (left), a retired college professor and active occupational therapist in mental health and cognitive behavior. Melba’s work has spanned the practices of psychiatry, pediatrics, school-based practice, gerontology, and long-term physical rehabilitation. Given her decades of experience working with clients of various backgrounds, Max asked Melba to share some thoughts on the mental health impacts of systemic inadequacies and racism. Here’s a conversation excerpt, which followed Max’s reference to “the insurance-doctor-client mental health pipeline, now the prison system.” Melba: The change in how healthcare is provided is thought to have been influenced over time by cost-cutting measures. Many individuals with mental illness are housed in prison systems secondary to the loss of public health care that was available at least 20 years ago. The point you made about the prisons appearing to become the mental health units is a concern expressed by others as well. There is concern about the increased privatization of mental healthcare and pricing the disenfranchised out of the opportunity to receive necessary treatment. You’ve also mentioned African-Americans as clients in mental healthcare. In many ways, this is quite a complex topic. When you consider the economic and social disenfranchisement of the African-American community for hundreds of years to present time; the systemic racial disenfranchisement in society, including healthcare, income; merely to exist and struggle with everyday discriminative challenges ... these are major factors that influence decisions about trusting hospitalization and healthcare equity. Additionally, there is a paucity of information about mental health treatment options and recovery. While there has been some noticeable progress in this area, the impact has been very minimal. The lack of and difficulty in accessing mental health services is a nationwide health care problem that unfortunately affects the minority communities far more than it should. The need for greater funding and education at the national and community level cannot be overemphasized. Personally, I am engaged in start-up efforts to develop a mental health ministry through my local church. I would like to do more to expose disenfranchised communities, especially African-Americans, to the benefits of mental health intervention; to reveal the health benefits and eliminate the myths and stereotypes associated with seeking mental health services. It would be great to help eliminate the perspective of mental illness being viewed as “another strike against oneself” because of ethnicity or socio-economic status. "The goal is to influence all of society, especially people of color, to perceive mental health as a 'user-friendly,' treatable illness." Having lived through generations of oppressive discrimination because of race, and with society’s seemingly negative attitude toward mental health … having a mental illness becomes an additional struggle for Black Americans and other people of color. The goal is to influence all of society, especially people of color, to perceive mental health as a “user-friendly,” treatable illness that is not to be treated as something to fear any more than hyper-tension, diabetes or cancer. The unfortunate reality and true difficulty is, among African-Americans the lack of equity is real in our society and in health care delivery. For generations, it has been a painful experience for many. So African-Americans face the challenge of having to deal with the potential mistreatment secondary to race and a diagnosis of mental illness. Max: How do mental health professionals broaden their scope? How do we advocate effectively when there is so much stigma assigned to Black communities? Melba: When society at large can truly embrace equity … that is my altruistic goal. If I had the answer to that question, I could change the world. Aside from greater funding for mental healthcare, how professionals are trained at classroom and clinical level is critical. Educating the public about the stigma assigned to mental health is also critical. Add these two factors to treating clients who happen to be African-American, Latino-American, Asian-American. … How do we effectively advocate for everyone, when there is so much stigma being assigned to the clients? Ethics, moral decency, healthcare justice, integrity, a sense of equity and fairness, eradication of the “isms” (systemic racism, religion, gender, sexual orientation, age discrimination) society has been working at equity among these for centuries … how far do you think we have come thus far? If your life involves discrimination for at least two of these, the intensity of treatment and the quality of the healthcare provider are paramount to the client’s success.
0 Comments
 Courtesy Tracey Robinson Courtesy Tracey Robinson In 2004, having seen depression affect their lives and communities, Tracey Robinson says she and her friend Stephanie Green wanted “people who look like us to have a place to come in and talk about it.” So they started Another Life Foundation, a 501c3 devoted to helping people of color battle mental illness and suicidal behaviors. Sixteen years later, they’re still at it: Stephanie continues to serve as executive director, and Tracey as board president. Through the years, Another Life Foundation has provided various services to people of color living with mental illness, from mentoring relationships to culturally competent counseling referrals to help accessing Social Security, Medicaid and Medicare benefits. During COVID-19, the foundation has created a Virtual Counseling Support Program and gone online with its Black Men’s Project. With support from NAMI Colorado Springs and other community entities, the Project brings conversations about mental health and wellness into barbershops and salons frequented by men and boys of color. Juaquin Mobley’s Community Barbershop hosted the Project’s first Wellness Summit back in January. The upcoming virtual summit, featuring five local speakers, will take place on Saturday, July 18, between 1 and 3 p.m. Registration is free, and attendees will have the chance to win prizes. As part of our ongoing blog series about the intersection of race and mental illness, we talked earlier this week with Tracey, a longtime health care professional, about what the foundation is working for — and against. NAMI: You were exposed to depression as a child, with two parents living with depression. How did that impact you personally, and specifically as a child of color? Tracey: Both of my parents were educated, and I came up as a middle-class child. So what do you do if you have parents who have good jobs and you look the part? No one's supposed to know [about mental illness in the family]. Because through history, there were the Jim Crow laws and segregation, and parents having to deal with the trauma of not being able to be Black. You wouldn't be hired if you had an Afro or things of that nature. So you don't add [other potential issues]. You have depression? What's that? What's that look like? It doesn't. It doesn't look like anything within the Black community, because you're taught to suck it up. You're not taught how to have coping skills. So that's the reason why we have Another Life Foundation: to let people know that it's OK to have a degree, to be educated, to be Black, and to have mental health [issues]. But you need to have coping skills, which are not given to you in the Black home. In Black homes, maybe you're not as fortunate to have parents who have good jobs. Maybe your parents are on welfare or you have a single parent, or they struggle. Then that looks different — maybe it's kind of the hip-hop culture. You deal with [illness] by “manning up,” you go get a tattoo, you pour out, you turn up, you drink liquor, you know what I'm saying? Then your coping mechanism is more destructive than productive. NAMI: You've mentioned a couple of the barriers you see standing between Black communities and mental health care. Are there others that you want to make sure people understand exist, that maybe they don't think of right away? Tracey: I think people at large do not think that trauma is a barrier between the Black community and mental health awareness and mental health access. Because when we process the trauma in our lives — seeing it in our homes — when we don't have the coping skills, we learn behavior. You saw Mom or you saw Grandma, but you don't know if they have schizophrenia or bipolar or whatnot. The resilience of the community of Black people on the whole is, "We march on." We've got to just keep standing, and keep marching. It's not OK to cry. And even if one does cry, that might be their only healthy way of dealing with what's going on. NAMI: Can you name some of the systemic problems that contribute to this dynamic? Tracey: If I'm performing at a level that's acceptable to my counterparts in white society, you don't see that I'm suffering from anxiety and depression, because of the resilience that I put up — the front. That's a problem. Feeding that back into the Black Men's Project, this is big in the Black men's community, because their anger and aggression from depression — that's the way it's manifested, by popping off. So then they have a higher risk of having police encounters. And in those encounters, it’s not, "Hey, are you OK?" You know, police aren't asking Black men if they have mental health issues, or if maybe they're having a bad day. It's just the buildup of the trauma over the years, of not knowing how to deal with it. Not having a mentor, not having someone you can go to talk to, not having the proper coping skills — and not seeing that there's anything wrong. Not having the avenues to say, "I need help," escalates you to other problems in your life. 'It's just the buildup of the trauma over the years, of not knowing how to deal with it.' NAMI: What you're describing goes beyond stigma. It's not just that people don't want to talk about their mental health issues, or that they’re feeling bad, it's that maybe they don't even recognize that the way they're feeling or reacting isn't healthy.
Tracey: Exactly. Because your mom or your dad — again, most of every behavior is a learned behavior, and from birth until the age of 7, all you're doing is downloading and processing how to respond. That’s how you’re trained to respond. No one said, "Hey, it's OK for you to cry." You didn't see your dad cry; you saw him go and hit your mom. So now you think that's the appropriate response. Or you didn't see your mom go and ask for help; she went and turned to a pipe. So, again, it begins to systematically become a cycle of abuse in the community. I did grow up with good things. Both my parents have degrees; my mother has a master's, my father had a bachelor's. My father also ran his own business. But he suffered. He had a sickness, and he didn't know how to deal with it. Therefore, he died at an early age, because he had cirrhosis of the liver, because he just drank. There's a better way. We don't want our young men to grow up thinking that the only alternative is to join the gangs, or the only alternative is to go and steal, or the only alternative is to go to jail. NAMI: What you're talking about is a whole lot of education and opening up conversation. Is there anything else that you feel is just essential to making positive change, making some headway toward getting mental health help to the Black community? Tracey: Let's just say that once we start opening the doors and it becomes OK to have a conversation, be patient. Because I've noticed that even within the community of mental health, it takes about 10 years, maybe longer in the Black community, to even come to grips that there is mental illness and to do the work and get the counseling. So patience and awareness is key. For more information on Another Life Foundation, visit anotherlifefoundation.com. For links to and information about additional resources dedicated to communities of color, see this page of our website. As part of our series on people who live with both racism and mental health issues, Max Maddox this week talked with Courtney Maupin, who has been a NAMI In Our Own Voice (IOOV) presenter in Denver for seven years. IOOV presenters work together in pairs to relate intimate, personal stories related to their own mental health. These are NAMI’s peer ambassadors to the public, representing the myriad ways mental illness can take hold of our lives — and be overcome with diligence and tenacity. Courtney has delivered her harrowing story, a bilateral struggle with race and mental illness, to audiences all over Denver, from inpatient psychiatric settings to the Crisis Intervention Team Training (CIT) program with the Denver Police Department. Here’s part of it, as told to Max. "I’m half black and half white. Our whole family has a history of mental illness. My mom did the best she could, being a single mom and a disabled veteran living with mental illness. When I was age 13, she just couldn’t handle it anymore. So I went into foster care for a while and then eventually I went to live with my aunt and uncle. They really tried to turn me against my mom, tell me she wasn’t sick, you know, put her down for everything she had gone through ... "But at age 16 I had my own job, I was paying all my own bills, I paid for my car, insurance, phone — you name it. I was getting my own food at school and from my part-time job working fast food. I started taking care of myself at 16, graduated high school at 16, and went to college at 17. Then I became pregnant at 18, and had my daughter at 19. That’s when my symptoms really started. "For the depression side of my bipolar type II disorder, it’s like I have these thoughts that just tell me, I’m not good enough, I should kill myself, Nobody cares about me, No one wants me around. I’m then sleeping all the time and can’t get the energy to get out of bed. It’s just a huge burden on my life. I don’t have interest in anything — it’s like, What’s the point of life? and Everything’s boring. "Then with the hypomania, it’s just impulsivity. You can’t control it, and thoughts come with it, too. Like you think, Oh it’ll work itself out, or Oh it's not a big deal … I’ll feel better if I go on a shopping spree. You just don’t have the impulse control to think things through. "Then I have mixed-episodes where I feel depressed, and with hypomania I can be really irritable, agitated. "My aunt and uncle weren’t around for me — they only wanted to talk about how 'I wasn’t that sick' or how they really didn’t think anything was wrong with me. I knew I had to find a better support system. That’s when I found the NAMI support groups. That was awesome, the Connection Recovery Support Groups, because I had an instant support system. The people that understood, that knew, checked up on me. I’m glad I had that. I now had that validation and I learned your worth doesn’t depend on anyone ... anyone else’s opinion. And those were the biggest things I took from intensive outpatient therapy, on top of getting on medication and attending therapy. "Recovery takes a lot of work, and that’s why I think people with mental illness are some of the strongest people out there. "Recovery takes a lot of work, and that’s why I think people with mental illness are some of the strongest people out there." "Just like anyone facing any physical illness, you have one more thing you have to overcome. But it’s such a different ballgame when your mind is working against you. For my symptoms of depression, some people think, 'Oh, depression is ’cause you’re sad,' or, 'You can be depressed and not be sad …' And you can go through grief — that closely emulates depression — but you don’t have a chemical imbalance.
NAMI is taking a hard look at its own struggles with diversity, and the knowledge that despite past efforts, we need to do more to reach further into the black and brown communities. Max asked Courtney what NAMI can do to be more inclusive — a question Courtney has grappled with deeply and personally. "In terms of mental healthcare in the Black community, and minority areas in general, it’s not there. The support is not there, the stigma is even higher. "So with NAMI, I just think it would be pulling in … minorities that we have already in the program, and allowing us to speak to these communities — and for people to see that there’s a different side to what they may have been accustomed to, or exposed to, with mental illness. You know, 'You need treatment' — let them know where treatment is available that works. Just like we do for everyone else in the community, but to really focus in on those areas. "I think NAMI does such a great job with mental health advocacy, support, education ... again I think it’s going into those areas that really need to hear it. "And we need to find more minority speakers. We need people who come from the Black culture who can be a testament to how they address mental illness and how they overcame it. We need IOOV in Spanish, and to get Hispanic people on board. We need to have them talk to the communities and reach out to support them. "We also need to vocalize it. … What are the mental health providers? Where do people go to get help? What are the places that can partner with our Law Line, where can we hold Family-to-Family courses, where can we hold Peer-to-Peer classes? And how can we do this in all areas of the community, and expand even more?" In his statement last week, NAMI national CEO Dan Gillison said that the organization is “early in our intentional Diversity, Equity and Inclusion journey.” Without question, that’s true of NAMI Colorado Springs as well. We’re a small, mostly white group with much to learn about the communities of color that we seek to better serve. One of the best ways to learn, of course, is to listen. So at this time of anger, anxiety, protest and reckoning, we’re talking about racism and mental health with people of color who live with mental illness.  Rochelle Johnson (All images courtesy of the artist) Rochelle Johnson (All images courtesy of the artist) Over the weekend, Max Maddox, an artist, author, In Our Own Voice state trainer and a project manager for NAMI’s Array Parity program, interviewed Rochelle Johnson, a fellow artist and Denverite. Years ago, Rochelle joined a Connection Support Group, where peers helped her better understand her schizoaffective disorder. “I was searching for some answers then about why this was happening to me, and how do I deal with it,” she says. “I met a lot of good people that were suffering from mental illness and were searching for the same thing.” Rochelle currently manages her illness with the help of the Mental Health Center of Denver and through drawing and painting, for which she was recently featured in Westword. Creating art helps her manage her stress and her symptoms, while also giving her a way to make statements about social justice. “I’m pretty sure change is on the horizon,” she says. Note: Questions and answers have been edited for length and clarity. Max: Can you share some of your story, Rochelle? Rochelle: After I graduated from art school, I moved to Seattle, in 1992. In 1999, I had my first break. It stemmed from working at an association there where I experienced a lot of hostility and stress, and a lot of it was about race. That really was my first attempt to work in corporate America, and my skin color presented a problem for most of the employees there — so much so that eventually I experienced my first break and they fired me, took my medical insurance away, and I was left to fend for myself. … I wouldn’t stay in the hospital in Seattle so [my parents] took me back to Denver and I got treated here, which is where I’m from. … The second break was when I worked at an art organization and I experienced the same kind of racism. This time I spoke up and left before it got too bad, but eventually I was hospitalized after I left that situation. Once again I had to start from zero and build myself back up. During all that time I was working on becoming an artist. So my journey is intertwined with art and hospitals. [Laughs.] Max: Can you say more about what your relationship with what the mental health system has been like? NAMI always wants to know how to work with the black community. This question about how to adapt our narrative of mental health to make sense to the black community … there’s always been this question since I started working with NAMI. Rochelle: I think it's all due to the location — where we are at. Colorado has fewer black people living here, per capita, than most major metropolitan areas. But there are black psychiatrists and black representatives that have their own thing going on around black mental health. I don't really know if it really has a lot to do with the church, or the fact that NAMI doesn’t really reach out to the community. It could be that right now, the community is all spread out. Five Points used to be a destination for people to find black people in general, their location, but not anymore. There is a percentage of black folks that deal with mental illness. Right now, during this time of the pandemic, people are grieving — and I guess that could be considered a mental illness, or not, just a mental wellness issue. People are grieving and may not know how to navigate that. Myself, I’m kind of numb. I’m numb to the fact that black men are being killed, black people are being killed, and the nation is doing nothing about that. There’s no response. So maybe it's time to talk about grief, the stages of grief, how you can manage that on a day-to-day basis. I’m managing my mental health issues right now, but I’ll tell you it's hard for me not to cry. Or even talk about the issues when I turned on my social media and saw a man’s life just be taken. How do I rationalize that? It was during the day! It was on social media. And the way the nation is dealing with it, I think is a good way, protesting, peaceful protesting, talking. Of course there’s always the rioters, but hell, if a certain group of people just want to focus on the rioting and the looting, I think there’s something wrong with them mentally. So, as a nation I think we need to talk about mental illness, mental well-being, how we can heal from this. Max: I love that you put this in terms of grief. I mean we’re talking about a dead man right now, we’re talking about dead people … I think that’s part of all our helplessness — and that part of the grief is to experience this helplessness, too. How has your studio work played into this: the social-political aspect of it, the healing aspect of it …? Rochelle: My work has always had a focus on the black community, how black people are doing now, how they spend their day-to-day time. Specifically I focus on black men, because I know they are more of a target than the rest of us. There is a longing, and an emotional connection, I have when they move into white spaces. I know at some point they will be villainized, because I go through that. How they react and how they relate in those spaces has always been something that I’ve captured in my paintings.
Right now my practice is going to be talking about both of the pandemics: COVID-19 and the killing of black people. I’ve always been one to paint everybody, but at this point I think the focus should be on black lives, because black lives matter. You can follow Rochelle on Instagram at @rochellejohnsonstudio. Check out and purchase her work, and find Rochelle’s contact information, at rochellejohnsonstudio.com. In the wake of the killing of George Floyd in Minneapolis, NAMI CEO Daniel H. Gillison Jr. issued the following statement:  Daniel Gillison Daniel Gillison “The effect of racism and racial trauma on mental health is real and cannot be ignored. The disparity in access to mental health care in communities of color cannot be ignored. The inequality and lack of cultural competency in mental health treatment cannot be ignored. “Our nation’s African American community is going through an extremely painful experience, pain that has been inflicted upon this community repeatedly throughout history and is magnified by mass media and repeated deaths. We stand with all the families, friends and communities who have lost loved ones senselessly due to racism. And, with more than 100,000 lives lost to the coronavirus pandemic — disproportionately from minority communities — these recent deaths add gasoline to the fire of injustice. “While there is much we need to do to address racism in our country, we must not forget the importance of mental health as we do so. Racism is a public health crisis. "Racism is a public health crisis." “As the nation’s largest grassroots mental health organization, it is our responsibility to serve all. While as an organization we are still early in our intentional Diversity, Equity and Inclusion journey and have much to do, we have renewed our commitment to our values. We continue to strive to deliver help and hope to all who need it. “NAMI stands in solidarity with everyone impacted across the country. You are not alone.” In the Pikes Peak region, we encourage anyone dealing with mental wellness challenges related to the anger and upheaval of this moment to contact our office at 719.473.8477. Beyond NAMI's own programmatic offerings, we can provide referrals to culturally competent mental health professionals in the area. As Dan said above, you are not alone.
 In 2014, Mary Ellen Benson joined the NAMI Colorado Springs board of directors because she was passionate about starting more conversations about mental health. Little did she realize the impact that would have on her own family. It’s not as though Mary Ellen was throwing her loved ones a huge curveball with her board membership; after all, she’s worked at AspenPointe since 2010, where she’s now vice president of community relations and business development. But when it comes to mental illness, she says, “There wasn’t conversation or really even awareness of it, on both sides of my family.” At least, not until she asked her mom, husband, kids, in-laws and others to come to the NAMI breakfast. “That really did a lot to compel their acknowledgment that we all have family members living with mental illness, yet people weren't talking about it,” she says. Now her clan comes to the NAMI fundraiser every year, many of them driving down from Boulder (where Mary Ellen spent her teenage years). “It's been an avenue to open up conversations that may have never happened,” she says. “My daughter even sang a song at one of the NAMI breakfasts that she had written about her own kind of day-in, day-out struggles with just living. Living as a teenager is hard. I'm not sure if she would have felt the freedom or the voice to do that, had it not been normalized and part of my family.” After six years as board secretary, Mary Ellen is cycling off due to term limits. Her departure means the loss of a great colleague and a gifted strategic thinker. (Consider: Before AspenPointe, Mary Ellen served for six years as HealthSouth Rehabilitation Hospital CEO, a position she earned at age 33.) So as a final board request, we asked Mary Ellen last week to share her thoughts about where NAMI’s been, and where it should go. How much did you know about NAMI when you joined the board? I really didn't know that much. I was overseeing an arm of AspenPointe where we were working a lot with the military. … Someone came in with, probably, a first-episode psychosis situation — kind of a young kid — and a clinician was trying to connect this family with NAMI. And I was like, "Tell me more.” Once she relayed its purpose, then NAMI started to pop up all over the place. When Lori [Jarvis-Steinwert, executive director], and Dan [Zarecky, former board president] asked me to join, my biggest push at the time was addressing the stigma around mental illness in the community. And there still is stigma — hear me that this has not been solved — but it was so brutal, particularly in the schools. This was before the rash of suicides. It was so not known for kids to say, "Oh, I'm going to therapy," or, "I'm going to my counseling appointment.” I also felt like there was such a disconnect between the business community and what was really going on within their organizations, with mental health challenges. So what got you excited about being a board member? Where did you see opportunity? It was pretty early on in that journey that we started participating in the National Dialogue on Mental Health. That was probably one of my proudest moments of really feeling like I was part of the community and trying to bring awareness to mental health. I was coming at it from a provider perspective. There wasn't this connection with users and providers and the community, a space of just honest, humble, open dialogue. It was usually providers versus users. I loved that work; that was an incredible campaign that we did. At the same time, we were also trying to move out of a working-board model into a governance board. It was really nice to be able to bring a voice forward that said, "We've got to figure out our business model, we've got to figure out sustainability.” You've long been active on boards. How have you decided which boards to get involved with? For me to give my time and energy to something, I need to feel personally connected and inspired by the work, and know that the goal of the organization is to make a difference. When I was on the American Heart Association board, we were doing a lot of work around awareness of women and their “Go Red For Women” campaign. I just really believed that there was so much focus on breast cancer awareness, and yet stroke and heart disease has such a huge impact on women, and we weren't even able to get the word out. Ironically, when I was a board member, my dad died of a sudden heart attack. That was a life-changing experience for me. He was a marathon runner, he didn't show any signs or symptoms, he was on no medications. His healthy lifestyle probably prolonged his life despite genetic heart issues. But it was one of those things that I could feel really proud of and say, "I would like you guys to support the Heart Association in honor of him." It's been a similar journey with NAMI, honestly. What’s your take on how NAMI and AspenPointe complement each other? AspenPointe has been in the community for a long time, over 150 years. NAMI is newer. And yet, we're both trying to work with folks who have had struggles for years upon years. How I've worked with trying to bring together NAMI and AspenPointe is asking, "How do we tell the story, and put a human face on people living with mental illness and their families?" We've been able to partner through some unique programs, like our Creative Expressions Art Therapy program, some of our programs with our peers, some of our programs around recovery. If you were referring somebody from AspenPointe to NAMI, and they didn’t know anything about NAMI, what would you say about it? I think the biggest thing is, "You're not alone. There are people just like you who can talk with you and help you understand how they've gone through their own journeys.” I've said to Lori so many times, "You can't separate the clinical provider side from the peer, or personal experience, side. If you try to, providers are going to fail.” Because you can only give folks health intervention one hour a week, whatever it is, and people are living this journey for the remainder: days, weeks, years. It's kind of like going to your primary care doctor who you see twice a year, and they tell you, "Lose 50 pounds, stop smoking, don't drink soda, start exercising.” In order to tackle any one of those things, you've got to find peer groups or support avenues. So what you might learn in therapy is made real, breathing and living through NAMI. "What you might learn in therapy is made real, breathing and living through NAMI." Even though so much is uncertain right now, do you have a sense of what a healthy NAMI might look like in five or 10 years?
I think there's going to have to be some private-public-nonprofit partnerships, and leveraging of resources to really further shared missions. Over time, particularly as we go through COVID and we have a recession and all of these pieces, we're going to have to look for other opportunities for revenue. So what does that look like? Can NAMI start to leverage the business community so that business and human resource programs are partnering in a financial sort of way? I think the shift is going to have to be moving upstream into a prevention or early intervention model. If you look at the American Cancer Society and the American Heart Association and some of these different illness-based organizations, they've all moved a lot more into health/wellness/prevention types of platforms. It’s about intervening early to help people stay as healthy as they can. What else would you want to say about your experience with NAMI or about the organization that you feel people should know? You can't go through a journey with NAMI without giving credit and love and acknowledgment to Lori. She's just, day in, day out, really helping change this conversation in our community. And I do think the people involved in NAMI — the volunteers, the board members, the staff — are a special group.  Collyn Florendo Collyn Florendo In 2013, still settling into her position as NAMI’s first executive director, Lori Jarvis-Steinwert walked into Bank of Colorado to play some hardball. NAMI had a CD with the bank, and she’d seen higher interest rates being paid elsewhere. Bank president Collyn Florendo was pretty new to his situation, too, having only recently relocated from Nebraska with his wife, Jackie. And he had a soft spot for nonprofits, having served on various boards and wanting to do more of the same in his new city. But after 30-plus years in business, mostly as a bank president, he wasn’t about to be hassled about his rate — especially knowing that Bank of Colorado had a history of sponsoring NAMI events. After Lori said her piece, she remembers, “He paused, looked out the window, and said to me, ‘How much money did Wells Fargo give you last year?’ I thought, ‘Point taken.’” Taken and very much appreciated. “He was obviously a character,” Lori says, “someone who was going to question and challenge me. He was quick on his feet. He had sort of a wry sense of humor. I knew those things would be great additions to the board.” Yes, Lori lost that day’s negotiation, but she won her next one, convincing Collyn to join NAMI’s board of directors. Over the last six years, he has shepherded NAMI’s financial growth from a $200,000 organization to a $500,000 one, providing steady leadership as treasurer and, in the last year, as president. This month, Collyn is term-limited off the board, but he has agreed to continue lending his business acumen as a member of NAMI’s Finance Committee. He recently sat down and talked about his experience with NAMI. What was it about Lori and the organization that made you want to be involved? I distinctly remember one of my first meetings at NAMI. There was a placard that showed all of the ways that mental illness shows itself, from eating disorders to addictions. I think I had an eating disorder in college: I was a wrestler in college and had to take some rather drastic measures to lose weight. So it was very clear to me how far-reaching mental illness is. I became involved, and I saw the efforts of Lori and her devotion to the cause. When I became a board member, I saw all the wonderful volunteers we have. It sold me on it. I saw how efficiently NAMI is run — at the time, it was a very small budget — and how all the people, from Lori to the volunteers, were really pouring their souls into the cause. It made me believe it was an organization I wanted to be part of and support the best we could. When you became engaged with the board, what role did you see that you could play to really help the organization? With my background being in finance, and having been involved in boards throughout the years … I hoped that maybe I could lend some insight to the finance side. I think I’ve always been willing to ask some of the tough questions and address some of the tough issues that need to be addressed. So that was really it. I didn’t know much about mental illness, but shortly after becoming involved with NAMI, I learned that my brother probably died of a mental illness, and my mother, and that I have had some other family members affected by it. Can you talk a little about your brother and how his experience affected you?
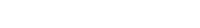
When he took his life, he wasn’t diagnosed. But now, after being with NAMI, I have no doubt that he was bipolar. He was a drug addict, so I watched that and how that affected his life. He eventually took his life when he was 45, so obviously that had a very profound effect on me. So I’ve learned more about mental illness and how it manifests itself in various ways. How did that experience affect your family? Well, I believe it killed my mother. I remember the phone call we got from law enforcement; it didn’t surprise me, because I knew he’d been struggling. But shortly thereafter, I think my mother suffered from depression. Eventually, she got cancer. She told me about it, but it was too late by then, by the time we found a specialist for her. I think she had just given up on life at that point. She had lost her oldest child, and I don’t think she ever recovered. Her official death is from cancer, but I think depression killed her. Over the six years you’ve been on the board, how have you seen people’s attitudes toward mental illness change? [Mental illness] has been so stigmatized by our society. It seems like it’s more accepted now. There should be no shame in it, and I think that’s how people are starting to perceive it. And I believe that’s due in part to the work of NAMI. If you were, say, at a dinner party, and you had to describe NAMI to somebody who knows nothing about it, how would you describe it? I would describe NAMI as being very compassionate, and fully devoted to helping those who are afflicted by mental illness in our society. … I think the passion and belief of the board members and our wonderful volunteers and Lori and our staff is as great as any nonprofit that I’ve served on. What are you most proud of, in the work you’ve done on the board? Helping with the finances has been very rewarding, to see the budget grow due to the great support of our NAMI staff and all the donors … and to see that we affect or help 2500, 3000 people throughout the year through a variety of programs at no cost to the people we serve. That’s been important to me, that through the generosity of the donors, we continue to be able to offer these programs at no cost. What is your greatest hope for NAMI moving forward? My greatest hope for NAMI in the future would just to be more visible. Ideally, I would like for NAMI to not be needed, but that’s a little idealistic. This is a disease that likely won’t go away. People continue to struggle with a lot of issues in their lives. … I think we are viewed as a leader in mental illness help. If we can continue to grow that presence, that would be my goal. Have you ever been told you’re too much? Too energetic, too idealistic, too different, too _____? We all have at some point. So we push it down, hide it from criticism, protect it by rejecting it. Yet those parts of us are still a part of us. They are waiting for permission to come out of hiding.
Now is the perfect opportunity to give them a chance. Nobody’s watching. Truly, everyone’s in hiding. As a result, couldn’t we all use your ”rebellion from boring” right now anyway? Bringing these parts of ourselves out of the shadows takes a lot less effort than hiding them. Living our truth releases the hold they have on us. Especially in times of crisis, our inner life can go neglected. Here's a short essay from NAMI volunteer Lelia Davis that asks us to stay tuned in.
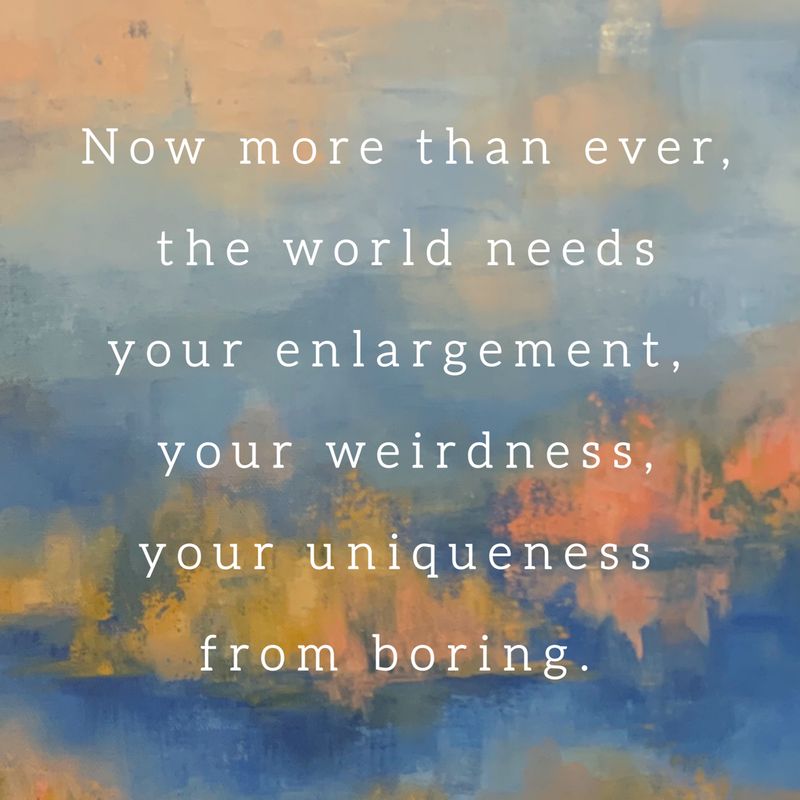
“Fine” is such a loaded word. Fine says, “I accept less.” Fine says, “I'm ok with not listening to what I want. I accept that what I want is not as important as what you want, or what is expected of me. I'll continue doing this because then I don't have to consider what I really want.” Many times, we must do things we don't choose, whether for work, family, our health, etc. Yet within these demands and obligations, we have the authority to choose. Do we choose the path of least resistance because it's familiar? Or do we take a risk and push the comforts of what we know? The answer lies within paying attention to what our bodies are telling us. Many of us have been told we're too emotional, yet our emotions are exceptional sensors. They are tuned into our desires, which are really just our basic needs. Our need to feel heard, seen, and understood. Ignoring these needs is living in the “Fine.” That catch in your throat, that flutter of your heart, that warmth that floods your entire body ... that's your emotion manifesting into something physical. Something that will get your attention. It's screaming, “I don't want to be fine! Pay attention to me! I want more!” Would you ignore that pleading if it came from your child, your best friend, your partner? Then why ignore ourselves? Why accept less when the plea comes from within? If we believe we are worthy of more, just like that loved one we would never ignore, then we can truly listen to ourselves and take action. We must believe that we are not only worthy of more, but that we're capable of more. What's more difficult, enduring what's “fine” for eternity, or risking the temporary discomfort of finding our “more”? leliadavisart.com  Locally, AspenPointe leaders have been working hard to recognize and respond to emerging community needs as the COVID-19 crisis unfolds. The region's largest mental health organization has confirmed that it is taking new patients for virtual care, and has posted a simple “Request appointment” button to the top right-hand corner of its homepage. If you don’t already have a mental health care provider, and feel like you could use one, it can’t hurt to make an inquiry. File under “Solidarity”: The Hartford Courant this morning published a poignant, but not-too-heavy, first-person piece from reporter Mike Anthony. He writes that though he’s fortunate, all things considered, “I’m just not rolling with the punches very well.” The Anxiety and Depression Association of America is making daily updates to a page of “Helpful Expert Tips and Resources” about coronavirus anxiety. It includes videos as well as blog posts that range in subject matter from mindfulness to parenting to responding to racism during the outbreak. Take care and be safe and healthy this weekend, everybody. Note: Edits were made to this post on Monday, March 30. |
AboutOccasional news items and tidbits from the office of NAMI Colorado Springs. Archives
June 2022
|
DONATE |
FIND A PROGRAM |
VOLUNTEER |
BECOME A MEMBER |
© National Alliance on Mental Illness - Colorado Springs. All rights reserved.
Pikes Peak homepage photo by NAMI volunteer Mike Pach.
Pikes Peak homepage photo by NAMI volunteer Mike Pach.




 RSS Feed
RSS Feed